
The Science of Body Temperature
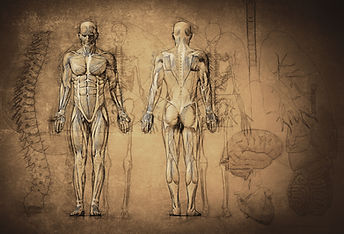
The core body temperature (CBT) of a healthy person is closely regulated within a normal range of 36.2°C to 37.5°C even when the ambient environmental conditions varies. When the body is too hot, the blood vessels in the skin dilate to allow excess heat to dissipate via the skin. In addition, the skin may sweat and there will be increased heat removal when the sweat evaporates from the skin surface. On the contrary, when the body is too cold, the blood vessels constrict, reducing skin blood flow and heat loss from the skin. The body may also start to shiver to increase heat generation from the muscles as well.
Since ancient times, physicians have understood that CBT is a vital sign of a person’s health. From primitive methods such as placing the hands to the forehead or neck, to the innovation of the mercury thermometer, methods to detect deviations in CBT have long been recognised as a key strategies to identify potential health concerns. Indeed, the monitoring of CBT can be of value in a variety of situations including infection monitoring, women’s health, heat-exposed occupations or sporting activities, and more.
Impact on Heat Stress on the Human Body
When the body’s thermoregulatory system is unable to keep up with the heat gained by the body, CBT may rise above the healthy range and the body experiences heat stress. Heat stress can reduce physical work capacity and motor-cognitive performances, thereby impacting health and productivity in heat-exposed situations including, but not limited to, sporting or occupational settings.

If left unchecked, heat stress can increase the risk of heat-related health concerns such as heat exhaustion, heat cramps and in the most severe instances – heat stroke. Heat-related health hazards is associated to increase morbidity and mortality especially during heat waves in the summer months. Individuals with chronic diseases such as type II diabetes and cardiopulmonary conditions can be more vulnerable to heat-associated health risk as well. In such instances, the continuous monitoring of CBT would be of great value as an indicator of heat stress and potential heat-related detriments.
Continuous Body Temperature Monitoring

The increased recognition of CBT as a health indicator over the years have spurred the development of more advanced thermometers based on a range of different technologies, including digital, electronic direct, predictive infrared (IR), and phase-change thermometers. These devices, however, only allow point-based measurement of CBT and cannot be used for continuous monitoring of CBT fluctuations and heat stress over a period of time.
Current CBT measurement systems that are established for continuous monitoring/recording of CBT are costly, single-use and mostly invasive. Examples of such continuous CBT monitoring systems are invasive temperature probes (typically oral, rectal or esophageal) or single-use telemetric temperature capsules, both of which are commonly used in research or high-risk surgeries, but not for consumer use.
The dearth in reliable consumer-based continuous CBT monitoring devices is the impetus that prompted the development of iTeMoS (intelligent Temperature Monitoring System). iTeMoS is an ear-based CBT monitoring system that enables CBT to be continuously recorded in an accurate, non-invasive, and most importantly, cost-effective way. It is in iTeMoS that we bring you the next evolution in continuous CBT monitoring technology as we strive to achieve what current technology cannot deliver – continuous CBT monitoring for ALL.
If you as excited as us, to find out more on our technology!
